JAMA. Viewpoint. The COVID-19 Pandemic and the $16 Trillion Virus. 12 October 2020.

The SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) pandemic is the greatest threat to prosperity and well-being the US has encountered since the Great Depression. This Viewpoint aggregates mortality, morbidity, mental health conditions, and direct economic losses to estimate the total cost of the pandemic in the US on the optimistic assumption that it will be substantially contained by the fall of 2021. These costs far exceed those associated with conventional recessions and the Iraq War, and are similar to those associated with global climate change. However, increased investment in testing and contact tracing could have economic benefits that are at least 30 times greater than the estimated costs of the investment in these approaches.Since the onset of coronavirus disease 2019 (COVID-19) in March, 60 million claims have been filed for unemployment insurance. Before COVID-19, the greatest number of weekly new unemployment insurance claims (based on data from 1967 on) was 695 000 in the week of October 2, 1982. For 20 weeks beginning in late March 2020, new unemployment claims exceeded 1 million per week; as of September 20, new claims have been just below that amount.
Recessions feed on themselves. Workers not at work have less to spend, and thus subsequent business revenue declines. The federal government offset much of the initial loss owing to the shutdown, which has averted what would likely have been a new Great Depression. But the virus is ongoing, and thus full recovery is not expected until well into the future. The Congressional Budget Office projects a total of $7.6 trillion in lost output during the next decade.1
Lower output is not the only economic cost of COVID-19; death and reduced quality of life also can be measured in economic terms. To date, approximately 200 000 deaths have been directly attributable to COVID-19; many more will doubtless occur. In the US, approximately 5000 COVID-19 deaths are occurring per week and the estimated effective reproduction number (Rt [ie, the average number of people who become infected by a person with SARS-CoV-2 infection]) is approximately 1. If these rates continue, another 250 000 deaths can be expected in the next year. Seasonal factors could increase mortality, although whether COVID-19 will display a large seasonal pattern is unknown. In addition to COVID-19 deaths, studies suggest increased deaths from other causes, amounting to almost 40% of COVID-19–related deaths. Thus, if the current trajectories continue, an estimated 625 000 cumulative deaths associated with the pandemic will occur through next year in the US.
Although putting a value on a given human life is impossible, economists have developed the technique of valuing “statistical lives”; that is, measuring how much it is worth to people to reduce their risk of mortality or morbidity. This approach has been used as a standard in US regulatory policy and in discussions of global health policy.2
There is a lengthy economic literature assessing the value of a statistical life; for example, in environmental and health regulation. Although no single number is universally accepted, ranges are often used. In environmental and health policy,3 for example, a statistical life is assumed to be worth $10 million. With a more conservative value of $7 million per life, the economic cost of premature deaths expected through the next year is estimated at $4.4 trillion.
Some individuals who survive COVID-19 are likely to have significant long-term complications, including respiratory, cardiac, and mental health disorders, and may have an increased risk of premature death. Data from survivors of COVID-19 suggest that long-term impairment occurs for approximately one-third of survivors with severe or critical disease.4 Because there are approximately 7 times as many survivors from severe or critical COVID-19 disease as there are COVID-19 deaths, long-term impairment might affect more than twice as many people as the number of people who die.
Given the predominance of respiratory complications among COVID-19 survivors, affected individuals may be like those with moderate chronic obstructive pulmonary disease, which has been estimated to have a quality-of-life disutility of approximately −0.25 to −0.35. Assuming a total reduction in quality-adjusted life expectancy, including length as well as quality of life, of 35% and taking into consideration the assumed value of a year of life yields an estimated loss from long-term complications of $2.6 trillion for cases forecast through the next year.
Even individuals who do not develop COVID-19 are affected by the virus. Loss of life among friends and loved ones, fear of contracting the virus, concern about economic security, and the effects of isolation and loneliness have all taken a toll on the mental health of the population. The proportion of US adults who report symptoms of depression or anxiety has averaged approximately 40% since April 2020; the comparable figure in early 2019 was 11.0%.5 These data translate to an estimated 80 million additional individuals with these mental health conditions related to COVID-19. If, in line with prevailing estimates, the cost of these conditions is valued at about $20 000 per person per year and the mental health symptoms last for only 1 year, the valuation of these losses could reach approximately $1.6 trillion.
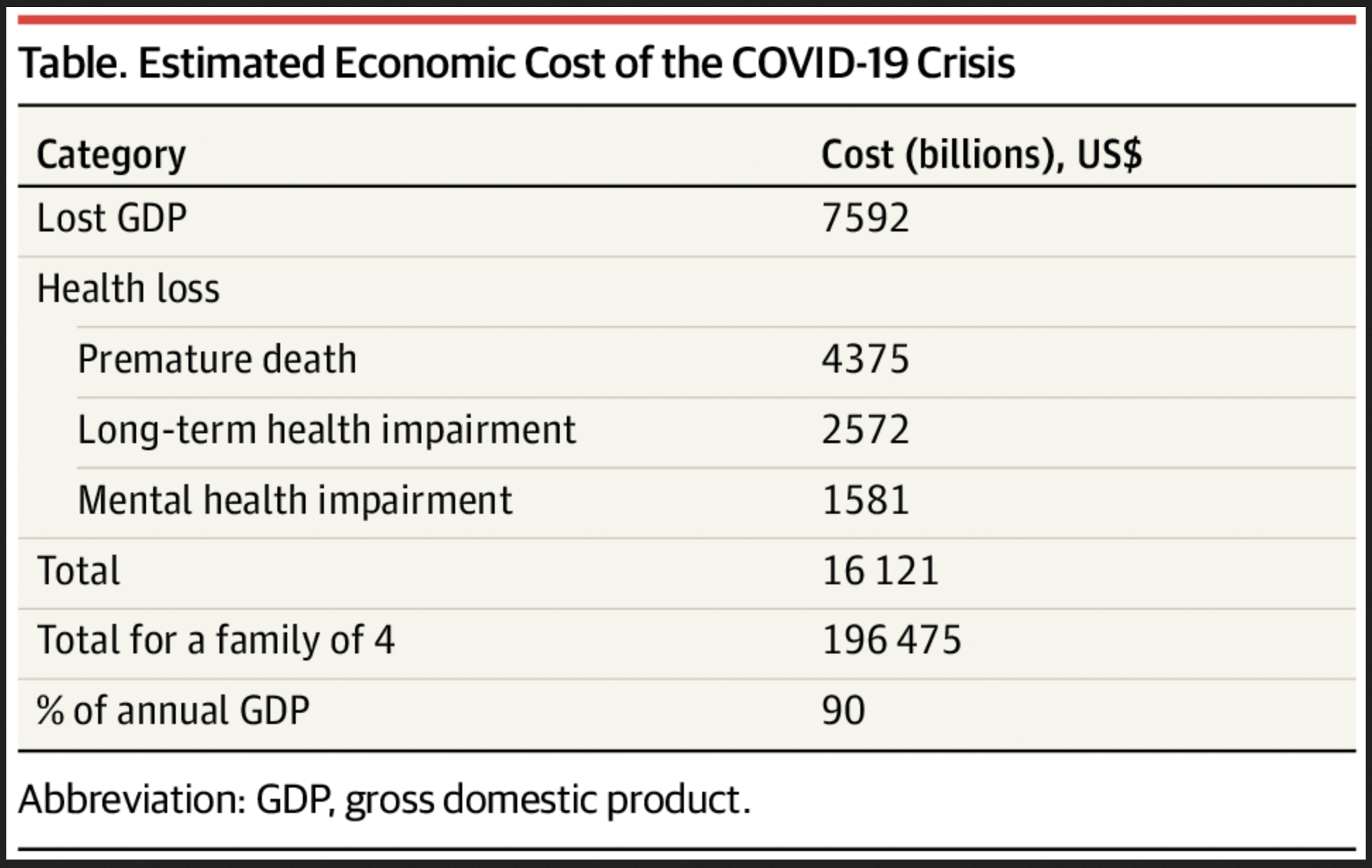
The estimated cumulative financial costs of the COVID-19 pandemic related to the lost output and health reduction are shown in the Table. The total cost is estimated at more than $16 trillion, or approximately 90% of the annual gross domestic product of the US. For a family of 4, the estimated loss would be nearly $200 000. Approximately half of this amount is the lost income from the COVID-19–induced recession; the remainder is the economic effects of shorter and less healthy life.